Q: Should I test my embryos using PGT-A test?
A: PGT stands for Preimplantation Genetic Testing. You might have also heard a similar test name, PGS, which stands for Preimplantation Genetic Screening. PGS is an older term describing a mostly similar test as PGT-A (more about PGT-A later). PGT is a test that a laboratory does to test whether an embryo has genetic abnormalities before it is transferred to a surrogate’s uterus. There are several types of PGT, but PGT-A is the most common test. The “A” in the test stands for Aneuploidy, which means having too many or too few chromosomes in a cell. Remember that a chromosome is a condensed DNA molecule and it holds the information necessary for proper growth and development. In every human cell other than an egg cell, a sperm cell, and a few other specialized cells, there are always 46 chromosomes. Specifically, there are 23 pairs of similar chromosomes, one pair from your mom, one pair from your dad.
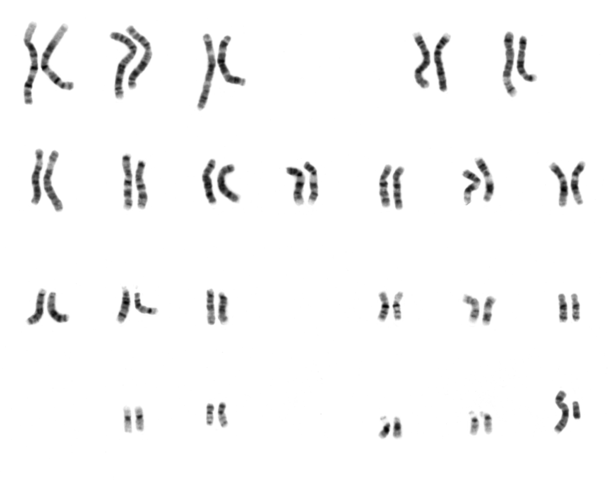
If there are too few chromosomes or too many chromosomes, the result might be a genetic disorder as the embryo develops into a fetus and a baby. There are only 200 to 300 cells in a 5-day or 6-day embryo (i.e. a blastocyst) and they eventually develop into a newborn with more than a trillion cells. Even if a few of the cells in an embryo contain an abnormal number of chromosomes, the resulting baby will have billions of abnormal cells. In most cases, all cells in an embryo have the same number of chromosomes because they all have developed from one fertilized cell in the beginning.
Some major genetic diseases that result from aneuploidy (an abnormal number of chromosomes) are:
- Patau syndrome (trisomy 13) – having three copies of the chromosome 13.
- Edwards syndrome (trisomy 18) – having three copies of the chromosome 18.
- Down syndrome (trisomy 21) – having three copies of the chromosome 21.
- Turner syndrome (45, X) – having only 1 X chromosome instead of the usual 2 X chromosomes or 1 X and 1 Y chromosomes.
- Klinefelter syndrome (47, XXX) – having three X chromosomes instead of the usual 2.
PGT-A aims to detect this kind of chromosomal abnormalities by sampling a few cells from your embryo and examining their chromosomes. If the number of chromosomes is abnormal, you will likely have to discard the embryo. Usually, a Mexican clinic would send a cell sample to a lab in the US specializing in this kind of tests and it might take 3 to 4 weeks for the result to come back.
PGT-A is usually done at a cost to the intended parents. Many agency programs make it optional and charges an extra fee of about $350 USD to $700 USD per embryo for it. However, PGT-A is not a cure-all for all potential genetic disorders. Consider these limitations:
- Inaccuracy in results: Like all other lab tests, PGT-A is not always 100% accurate. It may produce false positives or negatives. If the test result is wrong, you might discard embryos that could have developed normally or select embryos with unnoticed genetic issues.
- Mosaicism: PGT-A might not consistently detect mosaicism, where cells within the same embryo have different genetics. This inconsistency may cause misjudgments regarding an embryo’s health.
- Sampling error: The biopsy procedure of PGT-A, which involves extracting several cells from the embryo’s outer layer at the blastocyst stage, may not accurately represent the entire embryo. This is because other cells in the embryo may have different genetic makeup than the sampled cells (mosaicism, as described above) This can result in misleading test outcomes.
- Doesn’t detect all genetic abnormalities: While PGT-A evaluates the number of chromosomes, there are other kinds of genetic abnormalities even if the number of chromosomes is right. It fails to detect most single-gene disorders (that’s when one gene in a chromosome is abnormal) and structural chromosomal anomalies (that’s when one part of chromosome is missing or abnormal). Other genetic tests can detect these kinds of abnormalities, such as PGT-M (for single-gene disorders) and PGT-SR (for structural rearrangements).
- Impact on the embryo: The biopsy required for PGT-A introduces a minor risk of harming the embryo, potentially compromising its ability to implant and grow successfully.
Many intended parents including myself choose to have the embryo tested with PGT-A. Abnormal chromosomes is a significant cause of failed implantation, miscarriage, and development of genetic disorders. However, there is also a risk to the embryo when the doctor takes some cells from it. An intended parents should carefully consider the pros, cons, limitations, and cost of PGT-A and possibly consult with their doctor before making a decision.
Do you have any questions? Ask me and have your question and the answer featured on this website.

