After you have your high-quality embryos in your clinic in Mexico, it is time to find a surrogate, a woman who is willing to carry your fetus for you to term. This process involves several steps and you will likely need the help of a surrogacy agency or a clinic. Once an intended parent and a surrogate come to an agreement, surrogacy contract between the two parties is signed and the surrogate is prepared for embryo transfer procedure. It is possible, if you are willing and able, to find your own surrogate in an independent surrogacy journey, but it will take some time and skills, particularly if you are not in Mexico or if you don’t speak Spanish.
The following is the general steps taken by agencies to find, screen, and match a surrogate to an intended parent. Note that the exact process undertaken by each agency maybe different.
1. Surrogate Selection and Interview
A surrogacy agency in Mexico typically uses a surrogate network which has a database of women who want to become a surrogate. A surrogacy agency might also have their own database of surrogates who are pre-screened and ready to be matched. Your surrogacy agency will confirm the availability of the surrogate they think will be a good match for you and whether they want to be a surrogate for you. If the potential surrogate says Yes, the agency will send you the profile of the potential surrogate and / or arrange a video meeting between you as an intended parent and the potential surrogate.
As an intended parent, you have the right to carefully select a surrogate who will carry your fetus for 9 months. You have the right to ask questions, think over the proposed surrogate, and accept or reject the potential match. Particularly, many intended parents consider the following points when choosing a surrogate.
- Reliability and responsibility. Is the potential surrogate committed to helping you carry your fetus? Does the surrogate want to genuinely help you have a child, or is she only interested in money? If the potential surrogate is doing it only for money, she might not put care and love into carrying your child. You have to know she is responsible enough to fight temptation in drinking, smoking, getting a tattoo, or any other actions that may jeopardize the health of your child before and during pregnancy.
- Support system. Does the potential surrogate have a network of support from friends and family? This might be crucial for her well-being during the pregnancy. Also, do the potential surrogate’s family approve her choice of becoming a surrogate? If not, she might face conflicts during pregnancy and stress is not good for the fetus she will be carrying for you.
- Stable living situation. Is the potential surrogate in a stable home environment? Does she live in her own home with her family? Having a stable living situation, in my opinion, is very important. Some surrogates are in an abusive relationship, and that may force them to give up surrogacy in the middle of your journey. On the other hand, if she is in a stable family with lots of support, love and lack of stress can have a good impact on your unborn child.
- Lifestyle and home environment. Does the surrogate smoke or drink alcohol? If the surrogate drinks alcohol, can she refrain from drinking alcohol for 9 months? Does the surrogate’s home have pets? Is another member of her family at her home smoke?
- Previous successful birth. Has the surrogate given birth successfully in the past? Was the birth through surrogacy? If the surrogate has successfully given birth in the past, that means her ability to carry pregnancy to term is proven. Surrogates that have given birth previously are called experienced surrogates and they might require higher compensations.
- No chronic health conditions and work environment. Does the potential surrogate have chronic health conditions that require medications? Does the potential surrogate work in an environment that exposes her to toxic materials such as radiation or toxins? If so, will she stop working in that environment during pregnancy?
- Emotional stability and maturity. Is the potential surrogate emotionally mature and stable? You’ll want to select a surrogate who is emotionally mature so that you can count on her good decisions while she carries your child.
There are other, more objective surrogate selection criteria that most agencies rely on. These are:
- The surrogate has had an uncomplicated successful pregnancy previously, proving her ability to carry a child.
- The surrogate has not had too many pregnancies already.
- The surrogate has a BMI of less than 35, with 20 to 30 being ideal. BMI of 31 or more is considered obese.
- The surrogate is between 21 and 40 years old.
- The surrogate does not smoke or use drugs.
- The surrogate has a clean background check.
- The surrogate is mentally fit. An agency usually does a psychological screening to test this.
- The surrogate is medically fit. A clinic usually screens for signs of medical problems prior to her being officially assigned to you.
Note that in reality, you might not be able to find a perfect surrogate if the number of surrogates that your agency has access to is limited. It’s very much a trade-off between finding the right surrogate and enduring a longer wait time. Have your “must-have” criteria ready when you are reviewing the qualification of potential surrogates.
Once you and the potential surrogate agree that she will be your surrogate, it’s a match and you can move onto the next step.
2. Signing a Surrogacy Contract
A surrogacy contract between the intended parent(s) and their surrogate is a very important document. It outlines the expectations, responsibilities, and legal obligations of both parties. It also serves to memorialize the agreement that the intended parent(s) should have the full legal parentage of the child, not the surrogate. The surrogacy contract should be drafted by a lawyer specializing in surrogacy cases, and witnessed by an agency or clinic representative.
Specifically, the contract should have:
- Legal Terms: Surrogacy contracts address legal matters such as parental rights, medical decisions, and financial arrangements. It is ideal if the surrogate’s legal representative and the intended parent’s legal representative are different people so that there is no conflict of interest. However, this is not always the case in reality and it may depends on what kind of legal representation your agency provides.
- Medical and Health Terms: The contract specifies medical aspects of the surrogacy, including agreements on the number of embryos to be transferred, prenatal care, and the handling of potential complications or medical emergencies.
- Surrogate Compensation: The compensation schedule for the surrogate is clearly outlined. It also states who bears medical expenses and other related costs.
- Lifestyle Clauses: The contract should also include lifestyle considerations such as dietary restrictions, behavior during pregnancy, and communication with the intended parents.
3. Medical Testing of the Surrogate
At this point, the surrogate will have been medically screened to make sure she is fit to be a surrogate. However, some clinics may require the surrogate to undergo some routine medical tests to make sure she is healthy enough to undergo embryo transfer. This is an important part of the process as you wouldn’t want a surrogate with a medical problem carry your child for 9 months. Otherwise, unexpected complications may happen and the health of your fetus and/or your surrogate may become jeopardized.
The surrogate will undergo urine test and blood test to make sure they are free of drugs, infectious diseases, and other problems. In addition, a comprehensive physical examination is done to make sure the surrogate is healthy, and an ultrasound is performed to check the health of your surrogate’s uterus. Other checks may also be performed to make sure your surrogate is able to carry a fetus to term with minimal risks.
4. Health Insurance on the Surrogate
Most agencies purchase a health insurance on the surrogate that covers the health risks of the surrogate such as medical emergencies related to pregnancy and hospitalization due to complications. Note that this is different from an NICU Insurance for your newborn, and it covers only the health risks of the surrogate.
In Mexico, there is a mandatory 3 to 4 months waiting period from the start of a health insurance coverage during which the surrogate cannot be pregnant. In order for the surrogate to be properly covered during pregnancy, embryo transfer cannot happen until 3 to 4 months have passed since a health insurance is purchased for the surrogate.
- If an agency purchases a new health insurance policy for the surrogate after she is matched to you, there is a 3 to 4 months waiting period before embryo transfer can take place. During this time, necessary medical testing and/or medical preparation can be done.
- If an agency purchases a new health insurance policy for the surrogate before she is matched or if the surrogate already carries a health insurance, there might be little or no waiting time after the match. The surrogate can proceed to medical testing (if needed) and medical preparation for embryo transfer.
Note that because of this time restriction, some agencies choose not to purchase a health insurance for the surrogate. This would mean that the surrogate will not be covered if a medical problem arises during pregnancy. The intended parent may become responsible for unexpected medical costs arising from complications during pregnancy. It would also mean that you might not be able to purchase a newborn insurance to the surrogate’s health insurance once she is pregnant, if you are purchasing a newborn extension to the surrogate’s existing health insurance plan.
Newborn Insurance (NICU Insurance)
A newborn insurance or an NICU (neonatal intensive care unit) insurance is an insurance covering specifically your unborn child. In Mexico, if the surrogate who has a health insurance becomes pregnant, she can purchase a separate newborn insurance as an extension to her existing policy. This kind of insurance covers healthcare cost of the newborn once he or she is born. One of the biggest risk facing a newborn is premature birth. A premature baby may need to spend a considerable time in NICU in order for him or her to be well enough to be discharged. Also, babies born at term may face complications during birth. They might not able to breathe on their own, for example, requiring an extensive stay in NICU. The cost of NICU in Mexico can be as much as $1,000 USD to $2,000 USD a day (up to $15,000 USD per day in extreme cases). Without an NICU insurance or another kind of insurance covering the child, the intended parent will be on hook for these hospital charges.
When it comes to providing an insurance for your unborn child, there are 3 choices in general:
- Buy a policy extension to the surrogate’s existing health insurance, as mentioned above. The price tag is about $2,000 – $3,000 USD. This is an insurance from a Mexican insurance carrier.
- Buy an NICU insurance from your agency. Your agency may use a Mexican insurance carrier, another kind of carrier, or self-insure the risk. What “self-insure” means is that the agency will collect money from multiple intended parents and pay out when one of their newborns require an NICU stay. Essentially, the agency is acting as its own insurance company.
- Buy an international NICU insurance that has specific policy clause for surrogacy. An example of this is the Bupa Global Health Insurance. The insurance premium can vary widely. It can be as low as $5,000 USD, and as high as $40,000 USD or more.
5. Medical Preparation and Embryo Transfer
After you are matched with a surrogate and medical screenings are successfully completed, it’s time to transfer your embryo into your surrogate’s uterus. First, your fertility doctor will prescribe a number of medications to help thicken your surrogate’s uterine lining. In order for embryo transfer to result in successful pregnancy, the embryo has to “stick” to your surrogate’s lining instead of being washed away. Thicker uterine lining of about 7 to 8 mm has a better chance of making the embryo stick and grow compared to thinner uterine linings.
On the day of transfer, the doctor will use a catheter to slowly push the embryo directly into the surrogate’s womb. After the embryo transfer, the doctor will closely monitor the surrogate for signs of pregnancy such as mild cramping, missed period, and spotting. A beta hCG test is also performed to detect pregnancy. hCG is a hormone produced by the placenta shortly after the embryo attaches to the uterine lining. An elevated hCG level can be detected as early as 10 days after conception with a urine or blood test, and it rises rapidly in a healthy pregnancy. It continues to rise throughout the first trimester, then it declines. So, if the doctor detects rapidly rising levels of hCG over several weeks, the pregnancy has happened and is going well.
Not all embryo transfers end up successful. Read about the success rates, below.
How many embryos should / can I transfer?
Many fertility clinics give a choice of transferring one embryo at a time (single embryo transfer) or two embryos at a time (double embryo transfer). Transferring two embryos at a time means the doctor will inject 2 of your embryos at the same time into your surrogate’s uterus. Historically, doctors used to offer their patients a choice to transfer 3 or even 4 embryos at the same time to increase the chance of successful implantation. However, this kind of procedure is no longer performed today because there is a chance that 3 or 4 embryos all implant onto the woman’s uterine lining, resulting in triplets or quadruplets.
The chance of a single, excellent-grade embryo successfully implanting onto a surrogate’s uterine lining is about 65%. The rationale behind transferring two embryos at a time is to increase the chance of at least 1 embryo sticking to the uterine lining. However, if two embryos all implant onto the uterine lining, a twin pregnancy will result. Twin pregnancy is known to pose risk to both the surrogate and the newborns, including:
- Preterm labor and birth: Babies have a higher risk of being born with low birthweights and a greater chance of requiring NICU care.
- Gestational hypertension: A woman with twin pregnancy has a higher chance of developing high blood pressure during pregnancy.
- Anemia: A woman with twin pregnancy has a higher chance of developing anemia.
- Birth defects: Twins have a higher risk of being born with congenital abnormalities.
- Miscarriage: A woman carrying a twin has a higher chance of suffering miscarriage.
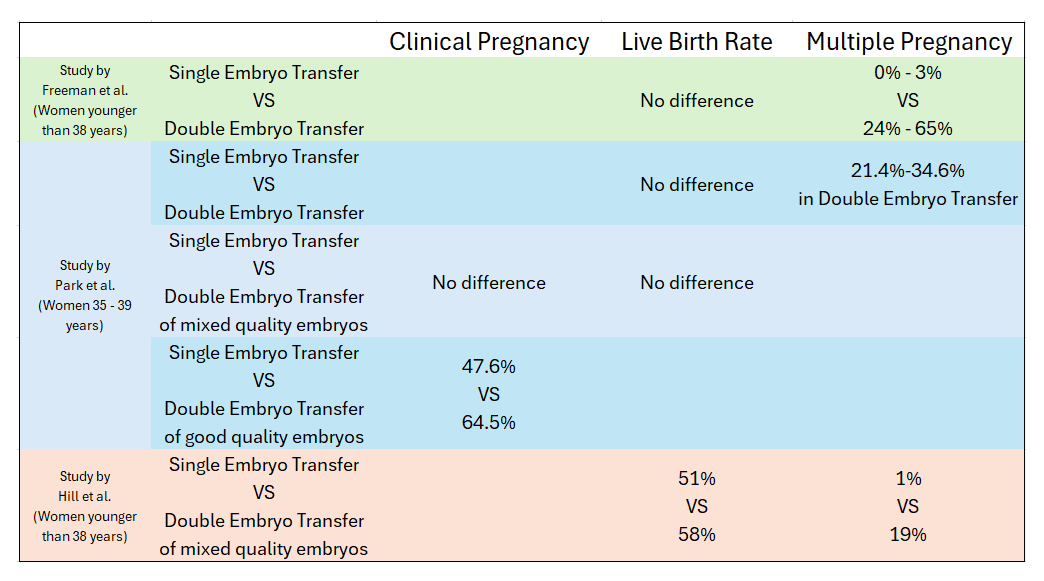
So, does double embryo transfers result in better pregnancy rates and live birth rates compared to single embryo transfers? Does double embryo transfers indeed result in higher risk of twin pregnancy? The research seems to be pretty conclusive; double embryo transfers may or may not result in higher live birth rates but do result in significantly higher chance of developing a twin pregnancy.
According to the review done by Kim and Matevossian, two studies done in 2019 suggest that the rate of multiple pregnancy was higher after a double embryo transfer compared to a single embryo transfer. This was true when doctors transferred two good-quality embryos. It was also true even when doctors transferred one good-quality embryo and one poor-quality embryo. This means that even a poor-quality embryo can successfully implant when transferred with a good-quality embryo. The result from these studies was confirmed by a more recent study done by Hill et al, which looked at a much larger sample size.
The study by Park et al. found that the pregnancy rate was higher when two good-quality embryos were transferred than when only one embryo was transferred. On the other hand, no difference in clinical pregnancy rate was found when mixed-quality embryos (e.g. one good, one bad) were transferred simultaneously. The three studies drew different conclusions for live birth rates.
In summary, while a double embryo transfer may increase the clinical pregnancy rates and live birth rates, it will increase the risk of twin pregnancy. For intended parents, twin pregnancy means increased risk that you’ll have premature birth. It also means that you’ll have to pay an additional compensation to your surrogate for carrying a twin, which can be around $10,000 USD. Additionally, you’ll also need to consider if double embryo transfer makes sense to you based on the number and quality of embryos you have. If you have only a couple of good embryos and a couple of average embryos, you might want to transfer the good embryos one at a time (i.e. two single embryo transfers) to maximize your chance of having at least one positive pregnancy.
What if my surrogate doesn’t become pregnant after an embryo transfer?
In general, the success rate of an embryo transfer is about 50% to 70%. Even if you use an excellent-quality (3AA – 6AA) embryo, the chance of clinical pregnancy is about 65%. That means it’s actually totally natural for an embryo transfer to fail. An intended parent might feel devastated after their first embryo transfer fails, but remember that many intended parents finally get a positive pregnancy after second or third embryo transfers.
When an embryo transfer fails, the fertility specialist assesses possible reasons why the embryo transfer failed and may adjust the surrogate’s medication or change the transfer protocols as he or she sees fit. You might also choose an embryo with a better grade, if you have one. Then, the surrogate is prepared for another embryo transfer.
When the embryo transfer fails three times, your agency or clinic will recommend you to change the surrogate. A partial compensation is paid to the surrogate, and depending on your contract, more surrogate screening or matching fees may have to be paid. The agency will attempt to match you with another surrogate, but usually, they will try to expedite this process.

