Q: What is embryo glue and should I use it for embryo transfer?
A: Embryo glue is a product that supposedly increases the the chance of successful implantation of an embryo when it’s transferred to a woman’s uterus. It aims to increase the chance of pregnancy and live birth whether you are transferring an embryo into your own uterus or your surrogate’s uterus. Embryo glue is a solution contains a substance called hyaluronan (also known as hyaluronic acid). Hyaluronan is a substance produced by cells of your body naturally, and is is involved in a variety of functions in your body. One of its functions is to form extracellular matrix in a mother’s womb, promoting embryo adhesion to the uterine lining.
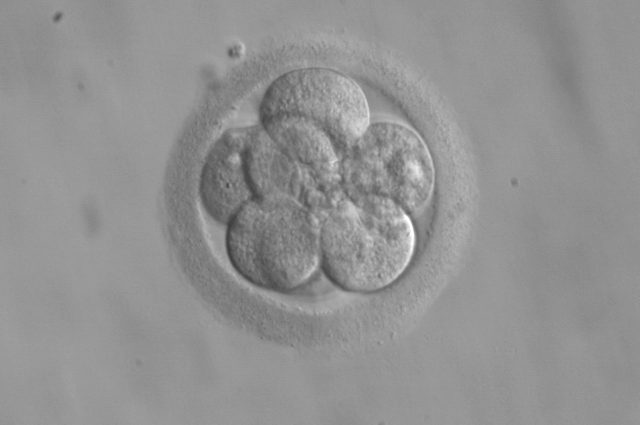
Before an embryo is transferred to the uterus, it is first dipped into an embryo glue solution, which contains albumin and other essential nutrients for the embryo in addition to hyaluronan. When the embryo is transferred to the uterus, hyaluronan increases the adhesiveness of the cells on the uterine lining, helping the embryo “stick” to it without being washed away.
Different clinics and embryologists have different opinions about embryo glue. Some doctors are confident that embryo glue can increase the chance of clinical pregnancy. Some are skeptical that embryo glue is useful at all. The cost of embryo glue is about $200 to $700 USD and intended parents are often given a choice to use it for their embryo transfer process.
While there were several studies published on the effect of embryo glue, one meta-analysis (a study that looks at many other studies) is often cited. It is a study published in 2020 by Heymann, Vida, Or, and Shoham in the Cochrane Library. It combines 26 studies with 6704 participants, and it includes only randomized controlled studies. Because each study uses different protocols and have a lot of other variabilities, the authors conducted statistical analysis to come up with the quality of evidence for each parameter studied. The notable results are:
- Live birth rate showed statistically significant improvement if high concentrations of hyaluronic acid was used compared to when low or no hyaluronic acid was used. The chance of live birth increased from 33% to between 37% and 44%. (20 studies, 4066 participants, moderate-quality evidence, meaning future research may change the author’s confidence in their estimate.)
- The effect on live birth rate was also present when only women with good prognosis were included. (6 studies, 1625 participants, moderate-quality evidence)
- Clinical pregnancy rate showed statistically significant improvement when high concentrations of hyaluronic acid was used. It improved from 40% in the control group to between 44% and 49% when hyaluronic acid was added in the transfer media. (17 studies, 5247 participants, moderate-quality evidence)
- The effect on clinical pregnancy rates persisted when only women with poor prognosis were included (2 studies, 288 participants, moderate-quality evidence), and when only women with good prognosis were included (6 studies, 1578 participants, moderate-quality evidence)
- Multiple pregnancy rates were higher when hyaluronic acid was used, with the rate increasing from 13% in the control group to between 16% and 21% in the group using hyaluronic acid (7 studies, 3337 participants, moderate-quality evidence)
The authors note that the increase in multiple pregnancy rates may be due to different protocols of transfer (i.e. single embryo transfer vs double embryo transfer) in different studies as well as the effect of hyaluronic acid increasing the implantation rate. Also note that the mean age of women in the studies ranged from 27.5 to 35.8 years, and how the results varied with the age was not provided. The authors also drew conclusions on other parameters such as miscarriage rate and adverse event rate, but these results were low-quality results, meaning future research will very likely change the author’s confidence in their conclusions.
One important consideration for people pursuing surrogacy is whether the result is relevant to embryos created from donated eggs or sperms. The authors did not provide an analysis based on whether the embryos are created from donated eggs or the participants’ own eggs. However, it does look at the results grouped by frozen-thawed embryos and fresh embryos.
- No evidence of improvement in live birth rates was found when only frozen-thawed embryos were included. (3 studies, 713 participants, moderate-quality evidence)
- Improvement in live birth rates was found when only fresh embryos were transferred. (6 studies, 2517 participants, moderate-quality evidence)
- No evidence of improvement in clinical pregnancy rates was found when only frozen-thawed embryos were included. (5 studies, 1056 participants, moderate-quality evidence)
- Improved clinical pregnancy rates was found when only fresh embryos were transferred. (10 studies, 2993 participants, moderate-quality evidence)
Frozen embryo transfer is typically performed for surrogacy cases. After embryos were created, graded, and frozen, your agency looks for and matches a surrogate to you. Once the surrogate completes the endometrial preparation step, a frozen embryo is thawed and transferred to the surrogate’s womb. The lack of evidence in live birth rates and clinical pregnancy rates may suggest that embryo glue is not as effective for embryos created using donated eggs, frozen, thawed, then transferred into the surrogate’s uterus.